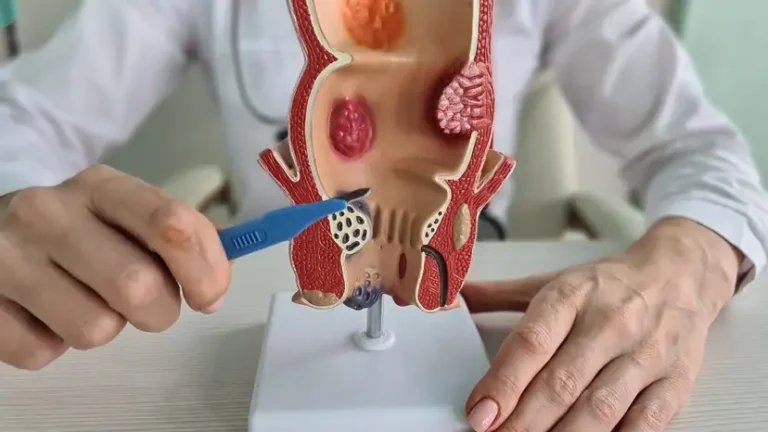
Anal fistulas are abnormal tunnels that form between the end of the bowel and the skin near the anus. They often develop after an infection in the anal glands, which can create a chronic abscess. Anal fistulas can cause pain, swelling, irritation, and sometimes drainage that makes daily activities uncomfortable. People living with this condition may experience embarrassment or fear of seeking help, but prompt evaluation by a colorectal surgeon is critical for proper management. Understanding how anal fistulas form, the symptoms to watch for, and the available treatment options can help patients make informed decisions about their care. Early recognition and treatment reduce the risk of infection spreading and prevent complications that may require more complex interventions. Modern surgical approaches prioritize both effective removal and preservation of anal function.
Understanding Anal Fistulas
Anal fistulas develop when an infection in the anal glands tunnels outward toward the skin. These infections often originate from blocked glands, leading to abscess formation. Over time, the abscess may drain spontaneously or through minor infections, creating a fistula tract. Common symptoms include persistent pain, swelling, recurrent abscesses, and discharge that may contain blood or pus. Patients may also notice irritation of surrounding skin or discomfort while sitting. Certain risk factors increase the likelihood of fistula formation, including Crohn’s disease, previous anal surgery, chronic diarrhea, or trauma to the anal region. Recognizing these symptoms early can help patients seek professional evaluation before the condition worsens.
When to Seek Medical Attention
Seeking prompt medical evaluation is essential for anyone experiencing persistent anal discomfort, drainage, or recurrent abscesses. Untreated fistulas can lead to ongoing infection, cellulitis, or even systemic illness. Chronic inflammation from a fistula may also damage surrounding tissues, making future surgical repair more challenging. Colorectal surgeons emphasize the importance of early consultation to prevent complications and optimize outcomes. Delays in care can increase the likelihood of multiple surgeries or prolonged recovery times. Patients experiencing fever, spreading redness, or severe pain should seek urgent attention to prevent the infection from escalating. Regular monitoring and timely intervention are key to effective management and long-term health.
Diagnostic Approaches for Anal Fistulas
Accurate diagnosis is critical for planning effective treatment. Colorectal surgeons usually begin with a detailed medical history and thorough physical examination. Imaging techniques such as magnetic resonance imaging (MRI) or endoanal ultrasound help map the fistula tract and identify secondary branches. In some cases, surgeons may use a probe to assess the depth and direction of the tract. These diagnostic tools ensure that the chosen treatment approach addresses all affected areas while minimizing damage to healthy tissue. Identifying the fistula’s relationship with the anal sphincter is especially important to prevent postoperative incontinence. Accurate diagnosis forms the foundation for successful repair and reduces the risk of recurrence.
Surgical Repair and Removal Options
Colorectal surgeons offer multiple surgical approaches to repair or remove anal fistulas, each tailored to the fistula’s complexity and location.
- Fistulotomy
Fistulotomy involves opening the fistula tract to allow healing from the inside out. This procedure is generally preferred for low fistulas that do not involve significant sphincter muscle. Advantages include high success rates and relatively straightforward recovery. Patients typically experience manageable pain and can return to normal activities within a few weeks. Risks may include minor bleeding and temporary discomfort during bowel movements. Fistulotomy is considered the gold standard for simple fistulas due to its balance of effectiveness and safety. - Fistulectomy
Fistulectomy removes the entire fistula tract rather than just opening it. This approach may be necessary for complex or recurrent fistulas. The procedure ensures complete excision of infected tissue but may involve longer healing times. Benefits include a lower risk of persistent or recurrent fistula formation. Postoperative care requires diligent wound management to prevent infection and promote healing. Fistulectomy is often combined with sphincter-preserving strategies to reduce the risk of incontinence. - Seton Placement
Setons are thin threads or tubes placed within the fistula tract to promote drainage while preserving sphincter function. This method is often used for high or complex fistulas. Setons can remain in place for weeks to months, gradually cutting through tissue or keeping the tract open for gradual healing. Patients must follow strict hygiene and wound care protocols during treatment. Seton placement reduces the risk of incontinence while controlling infection. It is commonly used as a staged approach before definitive repair. - Sphincter-Preserving Techniques
LIFT (ligation of intersphincteric fistula tract) and advancement flap procedures focus on closing the internal opening of the fistula without damaging sphincter muscles. These techniques are ideal for complex fistulas or patients at high risk for incontinence. Recovery may be longer, but the preservation of sphincter function improves quality of life. Surgeons may combine these approaches with other methods to ensure complete healing. Patients should be aware of the need for follow-up visits to monitor healing progress.
Non-Surgical and Adjunct Treatments
Not all fistulas require immediate surgery. Certain non-surgical approaches can complement treatment or provide temporary relief.
- Antibiotics may control infection and inflammation, particularly for patients with minor abscesses.
- Laser therapy offers a minimally invasive option to close fistula tracts while reducing recovery time.
- Platelet-rich plasma (PRP) therapy and other emerging treatments can promote tissue healing and reduce recurrence risk.
- Lifestyle adjustments, including dietary changes and improved hygiene, support the body’s healing process.
While these methods may help, surgical repair remains the definitive solution for most persistent or complex fistulas.
Recovery and Postoperative Care
Proper postoperative care is essential to ensure successful healing and prevent complications. Patients are often advised on pain management strategies, including prescribed medications or sitz baths. Wound care and hygiene are critical, especially in the first weeks following surgery. Dietary adjustments, such as a high-fiber diet and adequate hydration, help prevent constipation and strain during bowel movements. Regular follow-up visits allow surgeons to monitor healing and identify potential issues early. Patients should also learn to recognize warning signs, including unusual discharge, fever, or worsening pain. Recovery timelines vary depending on the procedure, overall health, and adherence to care instructions.
Preventing Recurrence and Maintaining Anal Health
Maintaining long-term anal health reduces the risk of fistula recurrence. Patients should identify and manage risk factors such as Crohn’s disease, chronic diarrhea, or repeated infections. Following recommended follow-up schedules ensures early detection if problems arise. Lifestyle changes, including a balanced diet, regular exercise, and good hygiene, support ongoing healing. Colorectal surgeons may also recommend periodic imaging for complex cases. Prompt treatment of any new abscesses or infections is crucial. Preventive care and proactive management contribute significantly to lasting results and improved quality of life.
Frequently Asked Questions
- How long does it take to recover from anal fistula surgery?
Recovery depends on the procedure type but generally ranges from a few weeks to a few months. - Can anal fistulas heal without surgery?
Small fistulas may sometimes close spontaneously, but most require surgical intervention to prevent recurrence. - What are the risks of incontinence after fistula repair?
Risk depends on the procedure and involvement of sphincter muscles. Sphincter-preserving techniques reduce this risk. - How do surgeons decide between fistulotomy and fistulectomy?
The choice depends on fistula complexity, location, and involvement of sphincter tissue. - Are there minimally invasive options for fistula treatment?
Yes, options like laser therapy, PRP treatment, and LIFT procedures can be minimally invasive alternatives. - What lifestyle changes can reduce the risk of recurrence?
Maintaining hygiene, high-fiber diet, hydration, and prompt treatment of infections are key preventive measures.
Takeaway
Anal fistulas can significantly impact quality of life, but modern colorectal surgery offers a range of effective repair and removal options. From traditional fistulotomy and fistulectomy to advanced sphincter-preserving techniques, patients have access to treatments that balance healing and functional outcomes. Early evaluation, accurate diagnosis, and careful postoperative care are essential for successful recovery. Non-surgical and adjunct therapies may complement surgical repair, while lifestyle adjustments support long-term health. With guidance from experienced colorectal surgeons, patients can navigate treatment options confidently and minimize the risk of recurrence. Understanding these options empowers patients to take control of their health and restore comfort and normalcy to daily life.